BW research into respiratory illness could lead to life-saving interventions
 BW
Public
Health
professors
continue
to
mine
historical
data
to
find
life-saving
answers
to
questions
about
respiratory
illnesses.
BW
Public
Health
professors
continue
to
mine
historical
data
to
find
life-saving
answers
to
questions
about
respiratory
illnesses.
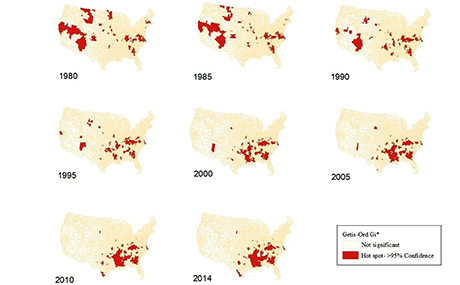
In the latest research published by a top-tier journal, Dr. Abolfazl Mollalo, with co-authors, Dr. Swagata Banik and Dr. Laura Hopkins, conducted pioneering work that predicts the location of hotspots of lower respiratory illness (LRI) in the United States.
Leading cause of death
For the first-of-its-kind study, published in the "International Journal of Medical Informatics," the BW researchers examined more than three decades of data on diseases of the lower respiratory tract, including bronchitis, bronchiolitis and pneumonia.
"Lower respiratory illnesses (LRI) have been classified as the seventh leading cause of death in the U.S., taking years off of life expectancy," explains Mollalo. "While several studies have been conducted in smaller geographic regions, no previous study examined geographic variations of LRI mortality rates and underlying factors across the U.S."
Novel data analysis
 For
the
BW
study,
Mollalo
analyzed
nationwide
historical
LRI
data
from
1980
to
2014
in
association
with
46
climatic,
topographic,
socio-economic
and
demographic
variables.
For
the
BW
study,
Mollalo
analyzed
nationwide
historical
LRI
data
from
1980
to
2014
in
association
with
46
climatic,
topographic,
socio-economic
and
demographic
variables.
Using novel methods, such as spatial statistics and machine learning techniques in a geographic information system (GIS) framework, the research has the potential to identify highly affected counties and to uncover possible reasons why lower respiratory mortality rates are higher in these areas.
Prediction and intervention to save lives
"Predicting
why
the
U.S.
counties
with
high
LRI
mortality
rates
cluster
geographically
can
be
helpful
to
further
reduce
mortality
in
these
regions,"
Mollalo
says.
"Despite
significant
efforts
for
control,
there
are
many
clustered
counties,
particularly
in
Georgia,
Kentucky
and
Virginia,
where
LRI
mortality
rates
have
remained
elevated
for
the
past
35
years."
"Overall,
there
was
a
historical
shift
in
hotspots
away
from
the
western
U.S.
into
the
southeastern
parts
of
the
country,
and
hotspots
were
highly
localized
in
a
few
counties,"
Mollalo
adds.
"Environmental
factors
contributed
most
strongly
to
these
hotspots,
while
economic
and
social
factors
seem
to
be
of
secondary
significance."
Higher spring temperatures and increased precipitation during winter are among the most substantial predictors of the presence or absence of the hotspots.
The findings imply that future budget and resources, such as vaccine allocation and additional healthcare workers, should be a priority for these areas.